Revolutionizing Post-Operative Care: AI Predicts Patient Outcomes with ECG Data
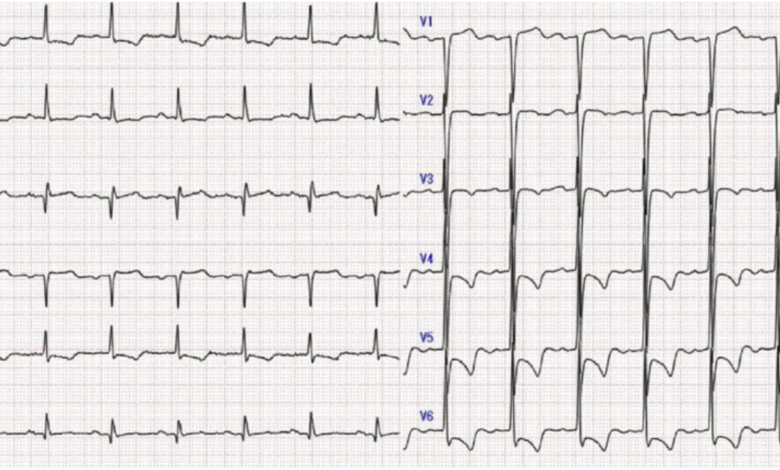
In a groundbreaking development, researchers at the Smidt Heart Institute at Cedars-Sinai, along with colleagues from Stanford University and Columbia University, have introduced an AI tool that accurately forecasts patient outcomes post-surgery. Published in The Lancet Digital Health, the study showcases a novel approach to utilizing pre-operative electrocardiograms (ECGs) in predicting post-surgical mortality.
The study encompassed patients from Cedars-Sinai, Stanford, and Columbia who underwent various surgical procedures, including open heart surgery and minimally invasive operations. The AI model, trained on pre-operative ECG data, marks a significant leap in the application of this 130-year-old diagnostic tool. Traditionally used to evaluate the heart’s electrical activity, the ECG now serves a pivotal role in this AI-driven prognostic approach.
David Ouyang, MD, a cardiologist at the Smidt Heart Institute and the study’s corresponding author, highlighted the uniqueness of this AI model: “This is the first electrocardiogram-based AI algorithm that predicts post-operative mortality. We’ve seen AI assess long-term mortality and individual diseases, but this application in forecasting surgical outcomes is a first, aiding the decision-making process for surgeries.”
The model’s predictive capability is noteworthy. By analyzing pre-surgery ECGs against post-procedure outcomes, it efficiently distinguishes between low and high-risk patients. Remarkably, those identified as high risk by the algorithm demonstrated a nearly nine-fold increase in post-operative mortality risk.
The AI tool addresses a crucial gap in current clinical practice. As Dr. Ouyang, also a member of the Division of Artificial Intelligence in Medicine at Cedars-Sinai, pointed out, existing clinical risk prediction tools are inadequate. This AI model could revolutionize how clinicians determine the suitability of patients for specific medical interventions.
Christine M. Albert, MD, MPH, chair of the Department of Cardiology at the Smidt Heart Institute and co-author of the study, emphasized the potential impact: “In cardiology, we have a range of life-saving procedures. Understanding risks, especially through a common diagnostic test like ECG, can significantly influence medical decisions.”
The researchers are now exploring how to transform this AI algorithm into a web application accessible to healthcare providers and patients, potentially changing clinical procedures and the utilization of prescription drugs. This advancement underscores the evolving landscape of medical technology, where AI and traditional diagnostic tools converge to enhance patient care and surgical outcomes.